Clinical manifestations of Syringomyelia is highly variable depending on the direction of widening the syrinx, transverse or longitudinal direction. Widening usually occurs towards the anterior of the spinal canal rather than to the right or left. Syringomyelia usually takes place slowly. Course of the disease can be up to many years. Acute symptoms will appear when it is on the brain stem (like syringobulbi).
Medical Health Information about Etiology, Clinical Manifestations, Diagnosis, Treatment and Therapy of Disease also Healthy Tips
Pathophysiology of Syringomyelia
Pathophysiology of syringomyelia is not widely known and most commonly used theory is the theory of Gardne , William and Oldfield .
Gardner's Hydrodinamic Theory
This theory suggests that syringomyelia is the result of a "water hammer" - like pulsatile transmission of Cerebrospinal Fluid ( SF) pressure, through a connection between the fourth ventricle and spinal canal centralis . Blockade originated from the foramen of Magendie.
This theory suggests that syringomyelia is the result of a "water hammer" - like pulsatile transmission of Cerebrospinal Fluid ( SF) pressure, through a connection between the fourth ventricle and spinal canal centralis . Blockade originated from the foramen of Magendie.
Classification of Syringomyelia
Classification of syringomyelia is still under debate, since the onset of the syrinx underlying pathogenesis is still under development and debate the experts.
Basically classification systems seen from:
Basically classification systems seen from:
Syringomyelia
What is Syringomyelia? for this session, it would be explained what Syringomyelia is. Syringomyelia is a chronic neurological syndrome that is pathologically found a syrinx in the spinal canal. Syringomyelia is a single lesion, tangible hole in the center of the central gray matter. Usually in the cervical or thoracic region. Syrinx can be connected with the central canal (canalis centralis) which called hidromyelia , or not related to the central canal, called syiringomyelia or be located in the central of the central canal called syringohidromelia. To facilitate the understanding of all the circumstances called syringomyelia .
Medical Treatment and Therapy for Amyotrophic Lateral Sclerosis
How to treat Amyotrophic Lateral Sclerosis? Here's explanation Medical Treatment and Therapy of Amyotrophic Lateral Sclerosis. No drug has been found to slow the progression of ALS. However, the Food and Drug Administration ( FDA ) has approved the first treatment for this disease is Riluzole. Riluzole is believed to reduce damage to motor neurons by decreasing the release of glutamate Clinical trials which performed to ALS patients, showed that administration of Riluzole can extend a patient's life until a couple of months, especially patients with difficulty swallowing.
Differential Diagnosis of Amyotrophic Lateral Sclerosis
There are several diseases that have symptoms and signs such as Amyotrophic Lateral Sclerosis. Here are some diseases that become differential diagnosis for, Amyotrophicl Lateral Sclerosis (ALS):
1. Another Motor Neuron Disease (MND)
a. Primary lateral sclerosis (UMN signs only)
b. Progressive muscular atrophy (LMN signs only)
c. Progressive bulbar palsy
1. Another Motor Neuron Disease (MND)
a. Primary lateral sclerosis (UMN signs only)
b. Progressive muscular atrophy (LMN signs only)
c. Progressive bulbar palsy
How to Make Diagnosis of Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis is difficult to be diagnosed since the beginning, because it may seem similar to some other neurological diseases. The medical experts caution after conducting a neurological examination tests to rule out other conditions, with signs of UMN and LMN in the same segment with asymmetrical anatomical localization is able to suspect the diagnosis of ALS. Examination that may be performed include:
Diagnostic Criterias for Amyotrophic Lateral Sclerosis
No test can provide a definite diagnosis of ALS, although the presence of interference at UMN and LMN in the body is very suggestive. The diagnosis of ALS is primarily based on signs and symptoms experienced by patients and through a series of investigations to rule out other diseases. Doctors dig deeply patient medical history and usually conduct a thorough neurological examination and to assess whether symptoms such as muscle weakness, atrophy of muscles, hyperreflexia, and spasticity worsened progressively. Because the symptoms of ALS can be similar to other illnesses, diseases that can be cured, appropriate tests should be performed to rule out other diseases.
Clinical Manifestations of Amyotrophic Lateral Sclerosis
Amyotrophic Lateral Sclerosis (ALS) symptoms are varies from one person to another according to the muscle groups that are affected by this disease. Tripping, dropping things, abnormal fatigue of the arms and / or legs, slurred speech, difficulty in speaking loud, uncontrollable laughing or crying, and muscle cramps and twitches all the symptoms of ALS. ALS usually starts first in the hand and will cause problems in dressing, bathing, or other simple tasks. It could develop into more on one side of the body and generally goes to the hands or feet. If start on foot, walking would be difficult. ALS can also start in the throat, causing difficulty swallowing. People with ALS do not lose their ability to see, hear, touch, smell, or taste. bladder and the muscles of the eye are not affected, nor desire and sexual function. The disease does not affect the mind of the patient.
Pathophysiology of Amyotrophic Lateral Sclerosis
The precise molecular pathways leading to degeneration of motor neurons in ALS is not known , but as with other neurodegenerative diseases , is likely to be a complex interaction between the various cellular pathogenic mechanisms may not be mutually exclusive include :
Etiology of Amyotrophic Lateral Sclerosis
The etiology is not known with certainly. ALS in 10% of cases derived autosomal dominant or autosomal recessive disorder which occurs on chromosome 2 or 21. Could be caused by a gene mutation for substances - toxic substances such as free radicals superoxide ions. Some are caused by an autoimmune process due to virus infection, especially poliovirus resulting in neuronal damage.
Amyotropic Lateral Sclerosis
 |
| Lou Gehrig |
Amyotropic lateral sclerosis is often called Lou Gehrig's disease, Maladie de Charcot or motor neurone disease is a progressive fatal neurodegenerative disease caused by the degeneration of motor neurons.
Multiple Sclerosis Disease-Modifying Therapies
Therapy was given only to minimize the incidence of attack, reducing the effects of attacks, and prolong remission. Disease-modifying therapies for early management of MS is currently available in the United States: intramuscular interferon beta-1a (Avonex), subcutaneous interferon beta-1a (Rebif), interferon beta-1b (Betaseron), and glatiramer acetate (Copaxone). The fifth agent, mitoxantrone (Novantrone), has been approved by the Food and Drug Administration (FDA) for the treatment of relapsing-remitting MS and secondary progressive MS is deteriorating.
Treatment and Therapy for Relaps Multiple Sclerosis
What are treatment and therapy for relaps Multiple Sclerosis?
1 . Adrenal corticosteroids .
Corticosteroids are the mainstay of therapy in reducing symptoms of acute relapses of MS. These agents work through immunomodulatory and anti-inflammatory effects, restoration of blood brain barrier and reduces edema. corticosteroids can also improve axonal conduction. Corticosteroid therapy shortens the duration of acute relapse and accelerates recovery. However, corticosteroids have not been able to increase the overall recovery of MS.
Medical Symptomatic Therapy for Multiple Sclerosis
Symptomatic therapy for Multiple Sclerosis
In addition to primary care, symptomatic therapy should also be considered such as:
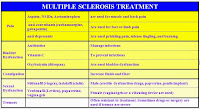 |
| Table Multiple Sclerosis Symptomatic Medicine |
In addition to primary care, symptomatic therapy should also be considered such as:
1. Spasticity
Mild spasticity can be reduced by stretching and exercise programs such as yoga, physical therapy, or other therapies. Medication administered when there are stiffness, spasm, or clonus on exertion or sleep state. Baclofen, Tizanidine, Gabapentin , and Benzodiazepines effective as antispasm agents.
Label:
Imuno Neurology
How to Make Diagnosis of Multiple Sclerosis
Diagnostic criteria commonly used is the McDonald’s criteria, which Multiple Sclerosis criteria with the original concept in 2001 and last revised in 2010. McDonald’s criteria emphasize the separation by time / disseminated in time two or more attacks) and separation by space / disseminated in space (two or more different diagnoses topis). Someone diagnosed definitely with Multiple Sclerosis when there is a separation of time and space that is clinically proven clinically or when evidence is incomplete but is supported by the investigation MRI, CSF or VEP).
Label:
Imuno Neurology
Clinical Manifestations of Multiple Sclerosis
What are Clinical Manifestations of Multiple Sclerosis?
Clinical Manifestations that appear according to the lesion area affected. There are several signs and symptoms that appear in multiple sclerosis:
a. Digestive and urinary dysfunction
b. The reduced perception of pain, vibration, and position
c. Fatigue and impaired mobility
d. Depression and cognitive or memory impairment
e. Vision and hearing problems
f. Tremor, hyperreflexia, spasticity, and positive Babinsky sign
g. Nystagmus, impaired coordination and balance.
Clinical Manifestations that appear according to the lesion area affected. There are several signs and symptoms that appear in multiple sclerosis:
a. Digestive and urinary dysfunction
b. The reduced perception of pain, vibration, and position
c. Fatigue and impaired mobility
d. Depression and cognitive or memory impairment
e. Vision and hearing problems
f. Tremor, hyperreflexia, spasticity, and positive Babinsky sign
g. Nystagmus, impaired coordination and balance.
Label:
Imuno Neurology
Multiple Sclerosis
A. Definition of Multiple Sclerosis
What is Multiple Sclerosis? Multiple sclerosis is an inflammation that occurs in the brain and spinal cord that attacks the white matter area and is a major cause of disability in young adults. Can be caused by many factors, especially the autoimmune process.
Label:
Imuno Neurology
Medical Treatment and Therapy of Hutington's Disease
Treatment and therapy of Hutington's disease can be classified into two: medically and non - medically. Some sources also suggest that gene therapy may also be an option in dealing with Huntington's disease. According to the Journal of Biological Chemistry, published in June 2009, explaining that a researcher has mengultur a cell that shows the formation of a gene RCAN known as RCAN-1L, these genes dramatically decreased in the brains of Huntington's disease. RCAN-1L was first discovered in the laboratory of the journal writer. Investigation of the study also showed an increase in the level of RCAN- 1L which later can save cells from the toxic effects of Huntington's disease, possibly sometime this gene may be one of the new therapies in dealing with Huntington's disease.
Label:
Degenerative Neurology
Diagnosis and Differential Diagnosis of Huntington's Disease
Diagnosis of Huntington's Disease is based on history, physical examination and investigation. From the history and physical examination found a family history of suffering from the same thing, usually occurs at the age of degenerative and psychiatric disorders and there is progressive cognitive decline. Found chorea movements are spontaneous movements that occur suddenly and redundant with the time and place of occurrence is erratic predilection.
Label:
Degenerative Neurology
Clinical Manifestations of Huntington's Disease
Clinical Manifestations of Huntington's Disease is characterized by impaired motor functions such as chorea movements, psychiatric symptoms, and dementia. Psychiatric disorder symptoms can appear as early symptoms before going to a real deterioration of cognitive function. Almost half of the patients with Huntington, experienced personality changes that disturb the people around him.
Label:
Degenerative Neurology
Huntington's Disease
 |
| George Huntington |
Huntington's disease is a hereditary disease which rare, with a medical condition which is characterized by the progressive degeneration of certain nerve cells in the brain , and is the result of a genetic defect that is carried on chromosome 4. Named after an American doctor " George Huntington " who first wrote this disease in 1872 .
Label:
Degenerative Neurology
Gait Impairment
A. Impaired Gait by Weakness
Impaired Gait due to weakness caused by the severe and chronic disease which causing extensive atrophy. This gait is not specifically indicate a neurologic disease or focal damage the nervous system. Form of gait disturbance imbalance (unsteadiness) and expect help. Patients seemed to sway to one side and the other, like ataxia. Patients want to lean on the chair looks to acquire holdings or against the wall. The movements are slow and seemed trembling knees.
Impaired Gait due to weakness caused by the severe and chronic disease which causing extensive atrophy. This gait is not specifically indicate a neurologic disease or focal damage the nervous system. Form of gait disturbance imbalance (unsteadiness) and expect help. Patients seemed to sway to one side and the other, like ataxia. Patients want to lean on the chair looks to acquire holdings or against the wall. The movements are slow and seemed trembling knees.
Label:
Neurology
Examination of Impaired Walking or Gait
During an investigation on pasen with impaired walking, required a thorough examination and assessment stage by stage .
It should be noted :
• symmetry and smoothness of movement
• stride length and width
• pace
• parts of the body, head, shoulders, arms, waist, hip, knee, heel and toe
• movement with related of the eyes, head and body
• noise generated from the road
• patient's job .
It should be noted :
• symmetry and smoothness of movement
• stride length and width
• pace
• parts of the body, head, shoulders, arms, waist, hip, knee, heel and toe
• movement with related of the eyes, head and body
• noise generated from the road
• patient's job .
Label:
Neurology
Physiology of Walking
A. WALK CYCLE
One cycle walking / gait from heel starts one foot on the floor (heel strike) until the next heel strike of the same leg, called the 100% total walking cycle. Certain points in the cycle can be observed.
a. 0%: heel strike at the beginning phase of standing (stance phase)
b. 15%: front foot touches the floor, also known as flat foot
c. 30%: the heel off the floor (heel off)
d. 45%: knee and hip flexed to accelerate the leg forward, in anticipation of the swing phase (swing phase) called a knee band
e. 60%: fingers off the floor, the end of the phase of the standing to initiate the swing phase, called the toe off. In mid-swing required dorsiflexion of the foot to prevent fingers touching the floor.
f. 100%: back heel touches the floor.
During the total run cycle, phase stands covering 60% and 40% of total cycle is swing phase.
One cycle walking / gait from heel starts one foot on the floor (heel strike) until the next heel strike of the same leg, called the 100% total walking cycle. Certain points in the cycle can be observed.
a. 0%: heel strike at the beginning phase of standing (stance phase)
b. 15%: front foot touches the floor, also known as flat foot
c. 30%: the heel off the floor (heel off)
d. 45%: knee and hip flexed to accelerate the leg forward, in anticipation of the swing phase (swing phase) called a knee band
e. 60%: fingers off the floor, the end of the phase of the standing to initiate the swing phase, called the toe off. In mid-swing required dorsiflexion of the foot to prevent fingers touching the floor.
f. 100%: back heel touches the floor.
During the total run cycle, phase stands covering 60% and 40% of total cycle is swing phase.
Label:
Neurology
Neurological Aspect of Walking
 In the process of walking
/ gait there is a complex process that is influenced by a number of
mechanisms of the body, and is the result of the collaboration of the
various types of reflex. Walk normally usually do not attract attention .
Walking impairment can be found in a variety of circumstances .
Mechanical factors such as diseases of the muscles, bones, tendons, and
joints play an important role in the occurrence of walking impairment .
In the process of walking
/ gait there is a complex process that is influenced by a number of
mechanisms of the body, and is the result of the collaboration of the
various types of reflex. Walk normally usually do not attract attention .
Walking impairment can be found in a variety of circumstances .
Mechanical factors such as diseases of the muscles, bones, tendons, and
joints play an important role in the occurrence of walking impairment .
Label:
Neurology
Medical Treatment and Therapy for Extrapyramidal Syndrome
General medical treatment and therapy for the extrapyramidal syndrome is patients treated with antihistamines such as difenhidramine , sulfas anticholinergics such as atropine or trihexyphenidil ( ( THP ) , 4 - 6mg per day for 4-6 weeks . Thereafter the dose reduced gradually , ie 2 mg every week , to see if the patient has developed a tolerance to the side effects of extrapyramidal syndrome . severe acute dystonia When the reaction had to be addressed quickly Beztropin generally given IV or IM diphenhydramine . awarded for acathisia anticholinergic and amantadine , and giving propanolol and benzodiazepines such as clonazepam and lorazepam .
Label:
Neurology
Clinical Manifestatations of Extrapyramidal Syndrome
The term extrapyramidal symptoms (EPS) refers to a group or reactions caused by the use of short-or long-term antipsychotic medication. This term may be made because many of the clinical manifestations skeletal muscle movements, spasms or rigidity, but the symptoms were out of control by corticospinal tract (pyramidal). However, the name is somewhat misleading because some of the symptoms (eg, acathisia) is not at all possible motor problems. Some extrapyramidal symptoms can be found simultaneously in one patient and overlap one another.
Label:
Neurology
Pathophysiology of Extrapyramidal Syndrome
Pyramidal arrangement
All the motor neuron impulses are channeled directly to the lower motor neuron ( LMN ) or , through its interneurons belonging to the group of upper motor neuron ( UMN ) . These neurons are residents presentralis gyrus . Therefore , it is called the motor cortex gyrus . They are in the fifth layer and each has a relationship with a particular muscle movement . The axons through contacting motoneuron motor cortex neurons that form the motor nucleus of cranial nerve and motoneuron in anterius medulaspinalis horn .
Label:
Neurology
Extrapyramidal Syndrome
Extrapyramidal syndrome is a condition that causes involuntary muscle movements or spasms that usually occur on the face and neck. This occurs when there is interference discharge arrangements and re-uptake of the neurotransmitter dopamine. An individual can suffer extrapyramidal syndrome as a result of head injury or Parkinson's disease, although the underlying cause is the side effects of antipsychotic drugs. Treatment is needed to prevent the worsening of symptoms, and treatment is usually directed action to identify and address the cause.
Label:
Neurology
Medical Treatment and Therapy for Cervical Root Syndrome
A. DRUG
Analgesics or muscle relaxants can be given in the acute phase. These drugs are usually given for 7-10 days. Types of drugs that are widely used are usually of salicylate or NSAID group. If things felt pain so severe, it is sometimes necessary also narcotic analgesics such as codeine, meperidine, morphine and even can also be given.
Analgesics or muscle relaxants can be given in the acute phase. These drugs are usually given for 7-10 days. Types of drugs that are widely used are usually of salicylate or NSAID group. If things felt pain so severe, it is sometimes necessary also narcotic analgesics such as codeine, meperidine, morphine and even can also be given.
Label:
Traumatic Neurology
Cervical Root Syndrome
 |
| Cervical Root Syndrome |
Cervical Root Syndrome is a condition caused by irritation or compression of cervical nerve roots, which is characterized by pain in the neck that spreads to your arm or depending on where the nerve roots are pressed.
Label:
Traumatic Neurology
Medical Treatment and Therapy for Epilepsy
Goal of epilepsy treatment
is to achieve optimal quality of life for patients. Principle that
pharmacological treatment of epilepsy:
1. AED (anti-epileptic drug) was started when the diagnosis of epilepsy is confirmed, there are at least two times a seizure in a year, the patient and family understand the purposes of treatment and possible side effects.
1. AED (anti-epileptic drug) was started when the diagnosis of epilepsy is confirmed, there are at least two times a seizure in a year, the patient and family understand the purposes of treatment and possible side effects.
Label:
Neurology
How to make Diagnosis of Epilepsy
To be able to diagnose a person with epilepsy can be done through anamnesis and clinical examination with EEG and radiological examination. However, if by chance saw the attack in progress, then epilepsy (clinical) can already be enforced.
Label:
Neurology
Clinical Manifestations of Epilepsy
Based on the type of seizure, there are several kinds of clinical manifestations of epilepsy. Here are the clinical symptoms and signs of epilepsy.
Label:
Neurology
Classification of Epilepsy
Classification of epilepsy
Epilepsy can be divided into three main sections include:
1. Grand Mal epilepsy
Grand mal epilepsy is characterized by the onset of excessive loose electrical charge of neurons throughout the brain areas in the cortex, in the inside of the cerebrum, and even in the brain stem and thalamus. Grand mal seizure lasts for 3 or 4 minutes.
Epilepsy can be divided into three main sections include:
1. Grand Mal epilepsy
Grand mal epilepsy is characterized by the onset of excessive loose electrical charge of neurons throughout the brain areas in the cortex, in the inside of the cerebrum, and even in the brain stem and thalamus. Grand mal seizure lasts for 3 or 4 minutes.
Label:
Neurology
Pathophysiology of Epilepsy
Etiopathologically, epileptic seizure can be caused by head injury, stroke, brain tumors, brain infections, poisoning, or even the growth of abnormal nerve tissue (neurodevelopmental problems), the influence of the genetic mutations that cause. Genetic mutations and cell damage in the physical injury or stroke or tumor will lead to changes in the function and structure of the regulatory mechanisms that lead to impaired neuronal growth-and plasticity at synapses. Change (focus) is what can lead to generation of electricity in the brain.
Label:
Neurology
Epilepsy
Epilepsy is a medical disorder and social or group, with characteristics unique. Epilepsy is usually defined as the tendency for seizures repeated. The word "epilepsy" comes from the Latin and Greek which means attack or disease arising suddenly. Epilepsy is a disorder which can occur in all species of mammals,, epilepsy is also very uneven around the world. Regardless of race, geography or social class, it can be occurs in both sexes, at all ages, especially in mass childhood, teenagers, and progressively increased when the elderly.
Label:
Neurology
Medical Treatment and Therapy of Tetanus
Three things to do in medical treatment and therapy of tetanus, there are:
1. Provide supportive care until tetanospasmin which binding with tissue, has been metabolized
2. Neutralize toxins in the circulatory system
3. Eliminating sources of tetanospasmin.
1. Provide supportive care until tetanospasmin which binding with tissue, has been metabolized
2. Neutralize toxins in the circulatory system
3. Eliminating sources of tetanospasmin.
Label:
Infection Disease Neurology
Diagnosis and Differential Diagnosis of Tetanus
DIAGNOSIS
Diagnosis is based on clinical findings and a history of immunization:
1. A history of the contaminated wound, but 20% can be no history of injury.
2. History is not immunized or incomplete immunization
3. Trismus, dysphagia, rhisus sardonicus, stiffness in the neck, back, and abdominal muscles (opisthotonos), pain and anxiety.
4. In the early neonatal tetanus complaint form can not suck
5. Episodic generalized seizures triggered by minimal stimuli and spontaneous where consciousness remains good.
Diagnosis is based on clinical findings and a history of immunization:
1. A history of the contaminated wound, but 20% can be no history of injury.
2. History is not immunized or incomplete immunization
3. Trismus, dysphagia, rhisus sardonicus, stiffness in the neck, back, and abdominal muscles (opisthotonos), pain and anxiety.
4. In the early neonatal tetanus complaint form can not suck
5. Episodic generalized seizures triggered by minimal stimuli and spontaneous where consciousness remains good.
Label:
Infection Disease Neurology
Clinical Manifestations of Tetanus
Clinical manifestations of tetanus varies from local muscle rigidity, trismus up strong spasms. Period until the onset of the initial symptoms of tetanus spasms known onset of disease, which affects the prognostic.
Label:
Infection Disease Neurology
Pathophysiology of Tetanus
How can Clostridium Tetani attack human body? let's discuss pathophysiology of tetanus. Clostridium tetani enter the human body through wounds usually in the form of spores. This Disease appears when spores grow into vegetative forms that produce tetanospasmin on the state of low oxygen tension, tissue necrosis or oxygen reduction potential.
Label:
Infection Disease Neurology
Tetanus
 |
| patient with tetanus |
Tetanus is a disease of the nervous system that is caused by tetanospasmin neurotoxin produced by Clostridium tetani, which is characterized by persistent tonic spasme accompanied by a clear and hard attack. Clostridium tetani enter the human body through wounds usually in the form of spores. Disease appears when the spores grow into vegetative forms produce tetanospasmin at low oxygen pressure conditions, or tissue necrosis oxygen reduction potential.
Label:
Infection Disease Neurology
Medical Treatment and Therapy of Trigeminal Neuralgia
 |
| Carbamazepine |
A. Medicamentosa
The most effective drugs are carbamazepine (Tegretol ®) 3-4X 100-200 mg a day depending on tolerance. These drugs, an anticonvulsant, is effective in most cases but causes dizziness and nausea in some patients while other patients on skin rashes and leucopeniasehingga to be discontinued. After a few weeks or months of administration, the drug can be stopped but must be given again if the pain recurs.
Drugs other than carbamazepine anticonvulsants can shorten the duration and severity of attacks. Medications such as this example phenitoin (300-400 mg / day), falproat acid (800-1200 mg / day), clonazepam (2-6 mg / day), and gabapentin (300-900 mg / day).
The most effective drugs are carbamazepine (Tegretol ®) 3-4X 100-200 mg a day depending on tolerance. These drugs, an anticonvulsant, is effective in most cases but causes dizziness and nausea in some patients while other patients on skin rashes and leucopeniasehingga to be discontinued. After a few weeks or months of administration, the drug can be stopped but must be given again if the pain recurs.
Drugs other than carbamazepine anticonvulsants can shorten the duration and severity of attacks. Medications such as this example phenitoin (300-400 mg / day), falproat acid (800-1200 mg / day), clonazepam (2-6 mg / day), and gabapentin (300-900 mg / day).
Label:
Facial Neurology
Diagnosis of Trigeminal Neuralgia
Trigeminal neuralgia should be distinguished with facial pain other. Medical examination and history of the symptoms must be done together other tests to rule out serious problems. Diagnosis based on an accurate anamnesis, clinical examination and clinical trials for know the exact location of stimulus triggers and pain during the examination. criteria diagnosis of trigeminal neuralgia customized with advanced by Headache Society classification Internatianal 1988.
Label:
Facial Neurology
Symptoms and Signs of Trigeminal Neuralgia
 |
| Symptoms and Signs of Trigeminal neuralgia |
Trigeminal neuralgia provide the following symptoms and signs
1. Neuropathic pain
Include severe paroxysmal pain , sharp, stabbing like, shot, electrocuted, hit by lightning, or burning a brief few seconds to a few minutes but less than two minutes, sudden and repetitive. Between attacks there is usually pain-free interval, or only mild dull taste.
Label:
Facial Neurology
Pathophysiology of Trigeminal Neuralgia
 Emphasis on the mechanics of blood vessels when the nerve root into the brain stem which is most often the case, while the portion above the trigeminal nerve / portio minor rare. Blood vessels in normal people do not intersect with the trigeminal nerve. This suppression can be caused by arterial or venous both large and small that may be just touching or bent on the trigeminal nerve.
Emphasis on the mechanics of blood vessels when the nerve root into the brain stem which is most often the case, while the portion above the trigeminal nerve / portio minor rare. Blood vessels in normal people do not intersect with the trigeminal nerve. This suppression can be caused by arterial or venous both large and small that may be just touching or bent on the trigeminal nerve.
Label:
Facial Neurology
Trigeminal Neuralgia
 |
| Patient with Trigeminal Neuralgia |
Trigeminal neuralgia is a disorder characterized by paroxysmal attacks of severe pain, and short in coverage of one or more nerves branch of the trigeminal nerve, usually without evidence of organic neurological disease. . This disease causes severe facial pain. This disease is also known as ticdoulourex or Fothergill's syndrome.
Label:
Facial Neurology
Medical Treatment and Therapy of HNP
Treatment
- Sleep for 1-2 hours on a hard mattress
- Exercise is used to relieve pressure or compression of nerve
- Drug therapy: muscle relaxants, nonsteroidal, anti-inflammatory and analgesic drug.
- Hot and cold therapy.
- Immobilization or brancing, using a lumbosacral brace or corset.
- Therapeutic diets to lose weight
- Lumbar Traction, may help, but usually Resides
- Transcutaneus Electrical Nerve Stimulation (TENS).
- Sleep for 1-2 hours on a hard mattress
- Exercise is used to relieve pressure or compression of nerve
- Drug therapy: muscle relaxants, nonsteroidal, anti-inflammatory and analgesic drug.
- Hot and cold therapy.
- Immobilization or brancing, using a lumbosacral brace or corset.
- Therapeutic diets to lose weight
- Lumbar Traction, may help, but usually Resides
- Transcutaneus Electrical Nerve Stimulation (TENS).
Label:
Traumatic Neurology
Clinical Symptoms and Diagnosis of HNP
Clinical Symptoms
a. Low back pain is intermittent (within a few weeks to several years). Pain spreading according to the distribution of the sciatic nerve.
b. The nature of pain changed from lying to sitting position, ranging from back pain and continued to spread to the back and then to the lower leg.
c. Pain intensified as the originator of such movements waist when coughing or straining, standing, or sitting for long periods of time and reduced pain at rest or lying down.
d. Patients often complain of tingling (paraesthesia) or numbness even decreased muscle strength in accordance with the distribution of the involved nerves.
e. Pain increases when the L5-S1 region (line between the two iliac crest) is pressed.
f. If left unchecked, it will slowly lead to lower limb weakness / leg
g. conus or cauda equina if affected, can occur defecation disorders, micturition and sexual function. This situation is a neurological emergency that requires surgery to prevent permanent damage function.
h. Habits of patients need to be observed, when sitting more comfortable then sitting on the healthy side.
a. Low back pain is intermittent (within a few weeks to several years). Pain spreading according to the distribution of the sciatic nerve.
b. The nature of pain changed from lying to sitting position, ranging from back pain and continued to spread to the back and then to the lower leg.
c. Pain intensified as the originator of such movements waist when coughing or straining, standing, or sitting for long periods of time and reduced pain at rest or lying down.
d. Patients often complain of tingling (paraesthesia) or numbness even decreased muscle strength in accordance with the distribution of the involved nerves.
e. Pain increases when the L5-S1 region (line between the two iliac crest) is pressed.
f. If left unchecked, it will slowly lead to lower limb weakness / leg
g. conus or cauda equina if affected, can occur defecation disorders, micturition and sexual function. This situation is a neurological emergency that requires surgery to prevent permanent damage function.
h. Habits of patients need to be observed, when sitting more comfortable then sitting on the healthy side.
Label:
Traumatic Neurology
Pathogenesis, Etiology and Risk Factors of HNP
PATHOGENESIS
HNP or herniation of intervertebral discs, which are often referred to as the Lumbar Disc Syndrome or lumbosacral radiculopathies is a common cause of lower back pain acute, chronic or recurrent. Protrusion, rupture, shifting is a term used in the disc nucleus which is pushed out. If the nucleus under pressure, while the nucleus is between two endplate of the vertebral body is confronted and surrounded by the annulus fibrosus pressure causes the nucleus pushed out, called the nucleus pulposus hernia.
HNP or herniation of intervertebral discs, which are often referred to as the Lumbar Disc Syndrome or lumbosacral radiculopathies is a common cause of lower back pain acute, chronic or recurrent. Protrusion, rupture, shifting is a term used in the disc nucleus which is pushed out. If the nucleus under pressure, while the nucleus is between two endplate of the vertebral body is confronted and surrounded by the annulus fibrosus pressure causes the nucleus pushed out, called the nucleus pulposus hernia.
Label:
Traumatic Neurology
HNP (Hernia Nucleus Pulposus)
 |
| Low Back Pain |
Waist is the back of the body, which help to support the body, from thorax to the superior and stomach. In anatomic, waist is the county, spine L-1 until all the bones of the sacrum and the surrounding muscles. Haunch has a very important function in the human body. Important functions, among others, make the body upright, movement, and protect several vital organs.
Label:
Traumatic Neurology
Medical Treatment and Therapy of Alzheimer's Disease
Treatment of Alzheimer's disease is still very limited because of the cause and pathophysiological still unclear. Symptomatic and supportive treatment as only gives a sense of satisfaction in patients. Stimulant medication, vitamins B, C, and E do not have any beneficial effect.
Label:
Degenerative Neurology
Clinical Diagnosis of Alzheimer's disease
There are several criteria for the are:
1. Criteria for diagnosis of suspected Alzheimer's disease include:
• Dementia established by clinical examination and the mini-mental status examination or some similar examination, and confirmed with neuro psychological test
• Obtained impaired cognitive function deficits> 2
• No disturbance of consciousness level
• Onset between the ages of 40-90 years, or often> 65 years
• There is no systematic abnormalities or other brain diseases
1. Criteria for diagnosis of suspected Alzheimer's disease include:
• Dementia established by clinical examination and the mini-mental status examination or some similar examination, and confirmed with neuro psychological test
• Obtained impaired cognitive function deficits> 2
• No disturbance of consciousness level
• Onset between the ages of 40-90 years, or often> 65 years
• There is no systematic abnormalities or other brain diseases
Label:
Degenerative Neurology
Clinical Symptoms of Alzheimer Disease
Onset of Alzheimer mental changes very slowly, so that patients and families do not know exactly when the disease began to appear. There are several stages of the development of Alzheimer's disease are:
Label:
Degenerative Neurology
Etiology and Pathogenesis of Alzheimer Disease
The exact cause is unknown. Some of the causes that have been made alternative hypothesis is metal intoxication, impaired immune function, viral infections, air pollution / industrial, trauma, neurotransmitters, deficit filament formation cells, heriditer pre-disposition. Alzheimer's disease pathology abnormalities basics consisted of neuronal degeneration, the specific area of brain tissue death resulting in impaired cognitive function with progressive loss memory.
Label:
Degenerative Neurology
Alzheimer's Disease
Alzheimer's disease is a neurological disease that are irreversible, due to this disease include: damage to memory, judgment, decision-making, and overall physical orientation in a manner of speaking. Diagnosis is based on neuroscience, the causes of dementia, can only be done by autopsy.
Label:
Degenerative Neurology
Medical Treatment and Therapy of Vascular Dementia
Therapies for vascular dementia is addressed to the cause, controlling risk factors (secondary prevention) and treatment of neuropsychiatric symptoms with regard to drug interactions. Other than that required multi-modality therapy for cognitive impairment and symptoms appropriate behavior.
Label:
Degenerative Neurology
Clinical Manifestations and Diagnosis of Vascular Dementia
Vascular dementia attack occurs suddenly, preceded by a transient ischemic attack (TIA) or stroke, the risk of vascular dementia 9 times in the first year after the attack and declined to 2 times as long as 25 years later. A history of risk factors, cerebrovascular disease should be aware of the possibility of the occurrence of vascular dementia.
Pathophysiology of Vascular Dementia
Vascular dementia or vascular cognitive impairment, is the end result of brain damage caused by cerebrovascular disease. The existence of multiple infarcts, lacunar infarction, myocardial single in certain areas of the brain, Binswanger's syndrome, cerebral amyloid angiopathy, hypoperfusion, hemorrhage, and a variety of other mechanisms to the pathogenesis of vascular dementia onset.
Etiology and Risk Factors of Vascular Dementia
ETIOLOGY
Vascular dementia is caused by the presence of cerebral vascular disease. The existence of a single infarct in a specific location, episodes of hypotension, leukoaraiosis, complete infarction, and bleeding can also cause cognitive disorders. Dementia syndrome that occurs in vascular dementia is a consequence of the lesion hypoxia, ischemia, or bleeding in the brain.
Vascular Dementia
Vascular dementia is a heterogeneous group of conditions that includes all of dementia syndromes caused by ischemia, hemorrhage, anoxic or hypoxic brain with cognitive impairment ranging from mild to the most severe, and not necessarily with a prominent memory impairment.
Diagnosis of Dementia
How to make diagnosis of dementia?
Dementia
is characterized by the presence of impaired cognition, function and
behavior, resulting in interference with work, daily activities and
social. Diagnosis is based on history, physical examination and neuropsychological assessment. History
/ interview include disease onset (acute / chronic), disease (stable /
progressive, improved), age at onset occurred, general medical and
neurological history, changes neurobehaviour, psychiatric history,
history-related etiology (such as infections, nutritional deficiencies , drug use, and family history). The physical examination includes vital signs, general examination, neurological and neuropsychological examination. Investigations include laboratory and radiological examinations.
Dementia
Dementia is a clinical syndrome that includes loss of intellectual functions and memory were so heavy that causes dysfunction of daily life - days. Dementia is a condition when a person experiences memory loss and other thinking power which significantly interfere with activities of daily living. Meanwhile, according to Lumbantobing (1995) is a set of symptoms of dementia degeneration in intellectual functioning, usually marked disruption of at least three functions namely language, memory, visuospacial, and emotional.
Medical Treatment and Therapy of Benign Paroxysmal Positional Vertigo
Management of BPPV include observation, medication to suppress vestibular function (vestibulosuppressan), canalith repositioning, and surgery. Primary election governance is observed, Because BPPV can own resolution in weekly or monthly. Therefore, most experts recommend that only observation. However, during the observation time of patients still suffer from vertigo. As a result, patients are faced with the possibility of falling when vertigo blaze while he was on the move.
Clinical Manifestations and Diagnosis of BPPV
Clinical Symptoms
BPPV occurs suddenly. Most patients are aware of the time they wake up, when to change position from lying to sitting. Patients feel dizzy spinning gradually diminished and disappeared. There is a lag between changes in head position with the onset of feeling dizzy spin. In general, feeling dizzy spinning arise very strong in the beginning and disappears after 30 seconds while its recurrent attacks become lighter. These symptoms are felt for days to months.
Pathophysiology of Benign Paroxysmal Positional Vertigo (BPPV)
In the inner ear there are three semicircular canals. Three semicircular canals are located in areas that are mutually perpendicular to each other. At the base of each Semicircular canals, there is a widened portion which called ampula. In ampula there cupula, is a tool to detect the movement of fluid in semicircular canals as result of head movement. For example, when someone turned his head to the right, the fluid in the right canal semicircularis will be left, so Cupula will deflecting towards ampula. Deflection is translated in a signal goes to the brain so that the sensation arises head turned to the right. With the availability of particles or debris in Semicircular canals, will reduce or even create cupula deflection towards the head instead of the actual direction of motion. It gives a signal that is not in accordance with the direction of head movement, so that arise in the form of vertigo sensation.
Benign Paroxysmal Positional Vertigo
Vertigo is a complaint which often encountered in practice, is often described as a sense of spinning, feeling shaky, unstable (giddiness, unsteadiness), or dizziness; description of the complaint is important to know in order not to be confused with headache or cephalalgia, especially because among the laity, the second term (dizziness and headache) are often used interchangeably.
Medical Treatment and Therapy of Vertigo
Because the causes of vertigo are varied, while patients often feel very annoyed with vertigo symptoms, often using symptomatic treatment. The duration of treatment are varied. Most cases of therapy can be stopped after a few weeks and here are some commonly used classes of drugs:
How to Make Diagnosis of Vertigo
How to diagnose Vertigo? How to make diagnosis vertigo use anamnesis and physical examination. Anamnesis includes clinical manifestations, family history, and treatment history. There is a family history of migraine, seizures, meniere disease, or deaf at a young age need to be asked and some medications can induce vertigo include ototoxic drugs, anti-epilepsy drugs, antihypertensives, and sedatives.
Pathophysiology of Vertigo
Vertigo arise if there is a disruption of the body's balance tool caused a discrepancy between body position (afferent information) actually with what are perceived by the central nervous system (central consciousness). The most important afferent arrangement in this system is, vestibular or balance, array, which is continuously delivers its impulse to the center of balance. Other arrangement that role is an optical system, and proprioceptive, poles connecting the poles vestibular nuclei with nuclei N. III, IV and VI, the vestibulo reticular and vestibulospinal arrangement. Information that is useful to balance the body would be arrested by the receptors vestibular, visual, and proprioceptive; vestibular receptors biggest contributing, that more than 50%, followed later visual receptors and the smallest contribution is proprioceptive.
Etiology of Vertigo
 |
| Vertigo |
Classification of Vertigo
Vertigo can be triggered by abnormalities in the central (brain stem, cerebellum, or brain) or peripheral (inner ear or vestibular nerve).
Definition and Epidemiology of Vertigo
What is Vertigo?
Vertigo is a feeling as if moving or spinning, or as if the objects around, are moving or spinning, which is usually accompanied by nausea and loss of balance. Definition Vertigo, is a hallucination, the environment movement, seemed to revolve around the patient or the patient seemed to revolve around the environment.
How to Diagnose Guillain–Barré syndrome
To make the diagnosis of GBS used criterion is the most commonly used criteria from the National Institute of Neurological and Communicative Disorder and Stroke (NINCDS), namely:
Label:
Imuno Neurology
Medical Treatment and Therapy of Guillain–Barré syndrome
In most patients, it can heal itself. Generally, treatment is symptomatic. Although it is said that it can heal itself, should be considered a long treatment time and number of disability or (sequelae) is high enough to keep the treatment should be given. The goal of therapy is to reduce the severity of disease specific and accelerate healing through the immune system (immunotherapy).
Label:
Imuno Neurology
Subscribe to:
Posts (Atom)






