Therapy was given only to minimize the incidence of attack, reducing the effects of attacks, and prolong remission. Disease-modifying therapies for early management of MS is currently available in the United States: intramuscular interferon beta-1a (Avonex), subcutaneous interferon beta-1a (Rebif), interferon beta-1b (Betaseron), and glatiramer acetate (Copaxone). The fifth agent, mitoxantrone (Novantrone), has been approved by the Food and Drug Administration (FDA) for the treatment of relapsing-remitting MS and secondary progressive MS is deteriorating.
Medical Health Information about Etiology, Clinical Manifestations, Diagnosis, Treatment and Therapy of Disease also Healthy Tips
Showing posts with label Imuno Neurology. Show all posts
Showing posts with label Imuno Neurology. Show all posts
Treatment and Therapy for Relaps Multiple Sclerosis
What are treatment and therapy for relaps Multiple Sclerosis?
1 . Adrenal corticosteroids .
Corticosteroids are the mainstay of therapy in reducing symptoms of acute relapses of MS. These agents work through immunomodulatory and anti-inflammatory effects, restoration of blood brain barrier and reduces edema. corticosteroids can also improve axonal conduction. Corticosteroid therapy shortens the duration of acute relapse and accelerates recovery. However, corticosteroids have not been able to increase the overall recovery of MS.
Medical Symptomatic Therapy for Multiple Sclerosis
Symptomatic therapy for Multiple Sclerosis
In addition to primary care, symptomatic therapy should also be considered such as:
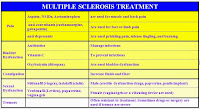 |
| Table Multiple Sclerosis Symptomatic Medicine |
In addition to primary care, symptomatic therapy should also be considered such as:
1. Spasticity
Mild spasticity can be reduced by stretching and exercise programs such as yoga, physical therapy, or other therapies. Medication administered when there are stiffness, spasm, or clonus on exertion or sleep state. Baclofen, Tizanidine, Gabapentin , and Benzodiazepines effective as antispasm agents.
Label:
Imuno Neurology
How to Make Diagnosis of Multiple Sclerosis
Diagnostic criteria commonly used is the McDonald’s criteria, which Multiple Sclerosis criteria with the original concept in 2001 and last revised in 2010. McDonald’s criteria emphasize the separation by time / disseminated in time two or more attacks) and separation by space / disseminated in space (two or more different diagnoses topis). Someone diagnosed definitely with Multiple Sclerosis when there is a separation of time and space that is clinically proven clinically or when evidence is incomplete but is supported by the investigation MRI, CSF or VEP).
Label:
Imuno Neurology
Clinical Manifestations of Multiple Sclerosis
What are Clinical Manifestations of Multiple Sclerosis?
Clinical Manifestations that appear according to the lesion area affected. There are several signs and symptoms that appear in multiple sclerosis:
a. Digestive and urinary dysfunction
b. The reduced perception of pain, vibration, and position
c. Fatigue and impaired mobility
d. Depression and cognitive or memory impairment
e. Vision and hearing problems
f. Tremor, hyperreflexia, spasticity, and positive Babinsky sign
g. Nystagmus, impaired coordination and balance.
Clinical Manifestations that appear according to the lesion area affected. There are several signs and symptoms that appear in multiple sclerosis:
a. Digestive and urinary dysfunction
b. The reduced perception of pain, vibration, and position
c. Fatigue and impaired mobility
d. Depression and cognitive or memory impairment
e. Vision and hearing problems
f. Tremor, hyperreflexia, spasticity, and positive Babinsky sign
g. Nystagmus, impaired coordination and balance.
Label:
Imuno Neurology
Multiple Sclerosis
A. Definition of Multiple Sclerosis
What is Multiple Sclerosis? Multiple sclerosis is an inflammation that occurs in the brain and spinal cord that attacks the white matter area and is a major cause of disability in young adults. Can be caused by many factors, especially the autoimmune process.
Label:
Imuno Neurology
Definition and Epidemiology of Vertigo
What is Vertigo?
Vertigo is a feeling as if moving or spinning, or as if the objects around, are moving or spinning, which is usually accompanied by nausea and loss of balance. Definition Vertigo, is a hallucination, the environment movement, seemed to revolve around the patient or the patient seemed to revolve around the environment.
How to Diagnose Guillain–Barré syndrome
To make the diagnosis of GBS used criterion is the most commonly used criteria from the National Institute of Neurological and Communicative Disorder and Stroke (NINCDS), namely:
Label:
Imuno Neurology
Medical Treatment and Therapy of Guillain–Barré syndrome
In most patients, it can heal itself. Generally, treatment is symptomatic. Although it is said that it can heal itself, should be considered a long treatment time and number of disability or (sequelae) is high enough to keep the treatment should be given. The goal of therapy is to reduce the severity of disease specific and accelerate healing through the immune system (immunotherapy).
Label:
Imuno Neurology
Clinical Manifestations of Guillain-Barré Syndrome
1. Weakness
Classical clinical picture is ascending weakness and naturally symmetrical. Lower limbs are usually affected first before the upper limbs. Proximal musculature may be involved earlier than the more distal. Body, bulbar, and respiratory muscles can be affected as well. Respiratory muscle weakness with shortness of breath may be found, developed acute and lasts for few days to weeks. Severity can range from mild weakness to tetraplegia with ventilatory failure.
Classical clinical picture is ascending weakness and naturally symmetrical. Lower limbs are usually affected first before the upper limbs. Proximal musculature may be involved earlier than the more distal. Body, bulbar, and respiratory muscles can be affected as well. Respiratory muscle weakness with shortness of breath may be found, developed acute and lasts for few days to weeks. Severity can range from mild weakness to tetraplegia with ventilatory failure.
Label:
Imuno Neurology
Pathophysiology of Guillain-Barré Syndrome
The mechanism of how the infection, vaccination, trauma, or other factors that precipitate the occurrence of acute demyelination in GBS is still not known with certainty. Many experts conclude that the nerve damage that occurs in this syndrome is through immunologic mechanisms. Evidence that the immunopathogenesis which is the mechanism that causes peripheral nerve injury in this syndrome are:
Label:
Imuno Neurology
Etiology of Guillain–Barré Syndrome
What are causes of Guillain–Barré Syndrome? Etiology is still not yet known with certainty and the cause is still a matter of debate. Some conditions / diseases that precede and possibly something to do with the Guillain–Barré Syndrome, among others:
Label:
Imuno Neurology
Guillain-Barre Syndrome
Guillain-Barre Syndrome (GBS) is an autoimmune neurological disease in rare cases, in which the immune system produces antibodies against its own nerve, resulting in damage of the nerve. Guillain-Barre syndrome is also called acute inflammatory demyelinating polyneuropathy that attacks the nerve roots both ventral and dorsal acute symptoms and lead to paralysis of the lower limbs begin and extends up the body and facial muscles.
Label:
Imuno Neurology
Medical Treatment and Therapy of Myasthenia Gravis
 |
| MG Treatment |
Diagnosis of Myasthenia Gravis
 |
Clinical Manifestations of Myasthenia Gravis
 |
| Ptosis in Myasthenia Gravis |
Pathophysiology of Myasthenia Gravis
When an action potential moves to motorneuron and reaches the motor end plate, the molecules of acetylcholine (ACh) is released from presynaptic vesicles, through the neuromuscular junction and then will interact with the ACh receptor (AchRs) in the membrane postsynaptic. AchRs canals open, allowing Na + and other cations into muscle fibers and cause depolarization. Persistent depolarization will converge into one, and if the accumulated depolarization is large enough, a meal will trigger an action potential, which moves along the muscle fibers to produce a contraction.
Myasthenia Gravis
What is Myasthenia Gravis? Myasthenia gravis is an autoimmune disorder caused by the presence of autoantibodies specific to human acetylcholine receptor (ACHR), which is concentrated in the synapses of the neuromuscular junction post. Myasthenia Gravis (MG) is a chronic, autoimmune causes muscle weakness and muscle fatigue slowly but progressively. If the patient is at rest, it is not long before muscle power will be restored. The disease is caused by the disruption of synaptic transmission at the neuromuscular junction.
Subscribe to:
Posts (Atom)



